Colon Polyps: Symptoms, Causes, and Treatment
Colon polyps are a common yet often ignored aspect of digestive health. While the word “polyp” may sound concerning, most are harmless and easily treatable when detected early. In this Blog, we’ll get to know about their symptoms, causes, and treatment options and proactive steps to protect your colon health and reduce the risk of complications.
Overview
Colon polyps are small outgrowths or lumps that form in the inner lining of the colon. Most of the colon polyps are harmless, but if left untreated, they may develop into colon cancer and can be deadly when found during the later stages.
Types of Colon Polyps
Adenomatous Polyps (Adenomas): The most common type of polyps that have the potential to become cancerous. They are mainly classified as tubular, villous, or tubulovillous adenomas based on their shape and histology.
Serrated Polyps: These can be hyperplastic or adenomatous. Some types, like sessile-serrated adenomas, have a higher risk of becoming cancerous.
Hyperplastic Polyps: Considered benign with a very low risk of turning into cancer.
Inflammatory PseudoPolyps: Often seen in people with IBD, these polyps themselves are not usually cancerous but indicate an increased risk of colon cancer due to the underlying inflammation.
Note- Inflammatory Pseudopolyps are not the real polyps or cause cancer, they are ulcers that have healed to form scar that looks like polyps. Chronic inflammation, such as Colitis, is the usual cause often related to inflammatory bowel disease(IBD).
What are neoplastic polyps and non-neoplastic polyps?
Based on the weather, a polyp can grow into a cancer or not. Polyps can be divided into
Neoplastic Polyp- It has the potential to evolve into a cancer; it includes
- All Adenomatous polyps
- Sessile serrated lesion
- Traditional serrated adenomas
Non-neoplastic polyp- Usually non-cancerous; includes
- Hyperplastic Neopolyps
- Juvenile polyps
- Inflammatory Pseudopolyps
How common are they in India?
Colon polyps are common in old age, affecting ~20% of adults and approximately 50% over the age of 50, and are also common in 6% of children. More common in western countries, the cases in India are rising, particularly in the younger population with one study showing 21% CRC patients younger than 40 years (read report here) In 2022, there were ~64,000 CRC (colorectal cancer) cases and ~38,000 deaths, indicating a high mortality rate. (Read journal)
What are the symptoms of colon cancer?
Most colon polyps don’t show any early symptoms; however, that is why the early screening is necessary. As the disease advances, it shows some symptoms. These include:
Blood in poop-A bleeding polyp could lead to blood in your poop when you wipe, indicating a sign of colorectal bleeding. This may also cause iron deficiency anemia, which can cause effects like weakness and fatigue.
Unexplained Bowel Changes- A sudden change in the bowel habits that doesn’t have an obvious cause, including diarrhea and constipation, excess mucus in poop could indicate colon cancer, consult with your doctor if symptoms lasts for more than a two weeks.
What are the Causes and Risk Factors?
- Family History – A mutation in the cells due to an error in the genetic code can lead to colon cancer and can be passed down through families, increasing the risk of colon polyps or colon cancer.
Genetic Disorders- Colon polyps are also associated with specific hereditary syndromes.
Familial Adenomatous Polyposis (FAP)- An inherited disorder characterized by the development of hundreds to thousands of polyps in the colon and rectum, often leading to cancer if untreated.
Hereditary Nonpolyposis Colorectal Cancer (HNPCC or Lynch Syndrome)- An inherited condition that increases the risk of colon cancer and other cancers, often at a younger age.
Peutz-Jeghers Syndrome- It is a rare genetic disorder causing polyps in the gastrointestinal tract and dark color spots all over the body.
Juvenile Polyposis Syndrome: A condition causing multiple polyps in the gastrointestinal tract during childhood or adolescence.
- Lifestyle
Diet- Diets rich in red and processed meats and low in fiber are associated with an increased risk of polyps. High-fat, low-fiber diets can alter the bacterial composition in the gut, contributing to polyp formation.
Smoking and Drinking- Tobacco use and Excessive alcohol intake are linked to an increased risk of developing polyps and colon cancer.
Obesity- Too much weight or being obese increases the risk of developing polyps and colon cancer.
Lack of Physical Activity- A sedentary lifestyle contributes to a higher risk of polyps.
Inflammatory Conditions- Conditions like Inflammatory Bowel Disease (IBD) cause chronic inflammatory conditions of the colon, such as ulcerative colitis and Crohn’s disease, which increase the risk of developing polyps and colon cancer.
- Age and Gender
Age- The risk of developing colon polyps increases as you age, particularly after age 50.
Gender- Men are slightly more likely to develop colon polyps than women.
- Type 2 Diabetes- Individuals with type 2 diabetes have an increased risk of developing colon polyps and colon cancer, possibly due to insulin resistance or associated metabolic changes.
- Hormonal Changes- Women taking hormone replacement therapy after menopause may have an increased risk of certain types of polyps.
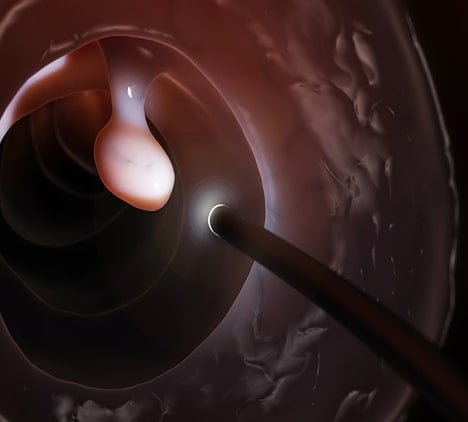
Diagnosis and Treatment
Colon cancer can be diagnosed primarily with the help of a colonoscopy, in which your healthcare provider looks inside your colon through a camera for detailed examination. Other tests include Imaging and blood tests that help in diagnosing the condition based on symptoms. Always consult with your doctor before testing.
Blood Test:
Complete blood count(CBC) test- This test checks for the complete blood profile to look for anemia due to chronic bleeding. A basic metabolic panel or Genetic testing helps you to find out the genetic mutation or any specific syndrome.
Stool tests- it includes fecal occult blood test that checks for blood traces in your poop to check for colon or colorectal cancer.
Imaging test
Virtual colonoscopy(CT colonography)- Produces 3d images of the rectum and colon through CT scans.
Capsule endoscopy– Uses a pill-sized camera to examine the colon.
Barium edema– A low GI X-ray examination that uses the barium liquid administered through the rectum, X-ray visuals are taken to examine the colorectal region.
Treatment
It includes colorectal surgery or polyp surveillance to check for polyps through microscopic examination for neoplastic and non-neoplastic polyps, It may take more than two weeks to result and diagnosis.
Procedure Includes:-
Polypectomy- It is a procedure done by a Gastroenterologist or a Colorectal surgeon to remove polyps. Some polyps may also require some special procedure, including Endoscopic Mucosal Resection (EMR), Endoscopic Submucosal Dissection(ESD).
Colonoscopy Surveillance- In case during Colonoscopy no neoplastic(Cancerous) polyps are found your doctor will closely monitor for other polyp to develop in every 5- 7 years by closely monitoring and screening depending on you individual risk factors.
Prevention
Regular Monitoring and Screening- Colonoscopy is the most effective method for detecting and removing polyps before they can turn cancerous. Guidelines generally recommend starting screening at age 50 for average-risk individuals, but earlier for those with risk factors.
Diet and Lifestyle Changes- Eating a high-fiber diet, reducing red and processed meat intake, maintaining a healthy weight, exercising regularly, and avoiding smoking and excessive alcohol can lower the risk of developing polyps.
A final thought
Colon polyps result from a combination of genetic, lifestyle, and environmental factors. While some risk factors, like genetics and age, cannot be changed, many lifestyle modifications and regular screenings can help reduce the risk and detect polyps early, improving the chances of preventing colon cancer. If you have risk factors or symptoms suggestive of colon polyps, it is essential to discuss with your healthcare provider and find the best cancer clinic for appropriate screening and preventive measures.