What Are the Signs That Immunotherapy Is Working?
Immunotherapy is an appealing organic therapy that can be used for numerous kinds of cancer cells. Nevertheless, different patients respond to immunotherapy in different ways, and the treatment is not effective for everybody. To figure out whether and exactly how well immunotherapy is functioning, a medical professional will continually keep an eye on the client’s progress.
Unlike chemotherapy and radiation treatment, which can create a rapid modification in the size of a growth that can be seen and gauged on imaging scans and with modifications in growth marker levels in the blood , immunotherapy can take longer to function. As immunotherapy medicines like Keytruda, Nivolumab, nd others gradually improve the all-natural cancer-fighting capabilities of the immune system, a growth might remain to expand. Furthermore, some individuals experience a postponed response to immunotherapy, while others experience a preliminary positive action followed by a relapse as the cancer develops resistance to the immunotherapy medicines. For every one of these reasons, it can take weeks or months to see a quantifiable response to immunotherapy.
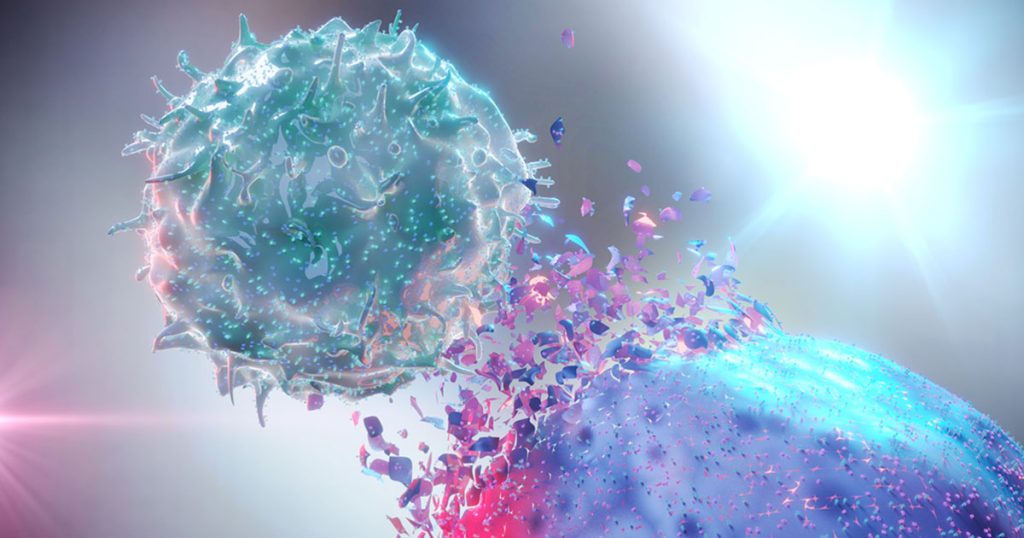
Immunotherapy is a wide category of cancer treatments that causes the body’s immune system to fight cancer cells. Cancer cells are different from typical cells because they do not proliferate normally. They quickly divide like an out-of-control copier that will not quit creating images.
These abnormal cells regularly transform, or mutate, helping them escape the body’s immune system, which shields the body from illness and infections. Cancer cells immunotherapy drugs are developed to alert the immune system concerning these mutated cells so it can locate and damage them.
How does the immune system work?
A key function of the immune system is to distinguish regular cells in the body from foreign cells.
The body’s immune system is constantly on patrol, like a police force charged with ridding the body of international invaders, such as viruses, germs, or fungi. Lymph nodes, which make up the majority of the body’s immune system, work as police headquarters throughout the body. White blood cells, consisting of lymphocytes such as “T cells,” battle infection and cancer cells. They are the law enforcement agents. When a foreign intruder is detected, the entire body’s immune system looks out via chemical signals, just as a police headquarters would radio a law enforcement agent to inform them regarding a problem.
The body’s immune system counts on receptor proteins on particular immune cells to spot the invaders. At specific checkpoints, when triggered or deactivated, these receptors allow it to distinguish between healthy and balanced cells and invading cells. The checkpoints are needed to maintain the body’s immune system from assaulting healthy cells.
Cancer cells do not activate an immune response due to the fact that they are the body’s very own cells that have mutated– so those once-healthy cells no longer act like typical cells. Due to the fact that the body’s immune system doesn’t recognize the difference, these unsafe cells can continue to expand, split, and spread throughout the body.
How does immunotherapy work to fight cancer?
Immunotherapies utilize various approaches to attack cancer cells. Immunotherapy kinds fall under three basic groups:
Checkpoint inhibitors, where cancer cells’ cell signals that trick the body’s immune system into thinking they’re healthy cells are interfered with, revealing them to be attacked by the body’s immune system
Cytokines, which are protein molecules that help control and regulate the body’s immune system that are manufactured in a lab and then infused right into the body in much larger doses than are produced naturally
Cancer cell vaccinations, which might reduce the risk of cancer cells by attacking viruses that cause cancer, or may treat cancer cells by stimulating the body’s immune system to attack cancer cells in a particular part of the body
Immunotherapy may be used alone or in combination with other cancer therapies, such as surgery, chemotherapy, radiation therapy, and targeted treatment.
What are a few of the immunotherapy drugs?
Existing checkpoint inhibitor drugs target the PD-1 and the CTLA-4 receptors. Typical checkpoint preventions include:
- Ipilimumab (Yervoy ®)
- Pembrolizumab (Keytruda ®)
- Nivolumab (Opdivo ®)
- Atezolizumab (Tecentriq ®).
Usual cytokines used in cancer therapy include:
- Interleukin-2 (IL-2).
- Interferons-alpha (IFN-alpha).
New immunotherapy medicines remain to be established.
How are immunotherapy drugs given?

The method of administration for immunotherapy medicines varies depending on the particular drug picked, yet the most typical administration courses are those listed here:
Oral: Pills or pills taken by mouth.
Intravenous: Drugs that are administered through one of the person’s blood vessels.
Intravesical: Medications are provided right into a client’s bladder.
Topical: Medications that come in a lotion or cream that the client puts on the skin.
Tumor-agnostic therapies
The United States FDA has also authorized immunotherapy to treat cancers with particular hereditary features, no matter where in the body they come from. These therapies, called tumor-agnostic treatments, might be used to deal with these malignancies:.
Strong lumps with microsatellite instability-high (MSI-h) or mismatch repair work shortage (dMMR): These tumors may have unsteady hairs of DNA or are incapable of repairing DNA damage.
Solid lumps with high tumor mutation burden (TMB-h): These growths have cells with a high variety of gene mutations, which may make them more likely to react to immunotherapy.
Signs immunotherapy is working.
After immunotherapy is given, the treatment group looks for signs that the medicines are working. Commonly, one of the most vital indications that the medicine functions is that the growth is either smaller or is remaining stable without a boost in size.
Some individuals believe that experiencing negative effects is a sign that immunotherapy is working, but not all patients with successful immunotherapy therapy experience negative effects from the medicines.
What are immunotherapy side effects?
Immunotherapy might create a selection of negative effects– lots of are flu-like symptoms– consisting of:.
- Fatigue.
- Queasiness or throwing up.
- Mouth sores.
- Looseness of the bowels.
- High blood pressure.
- Fluid accumulation, generally in the legs.
- High temperature or chills.
- Discomfort or weak point.
- Migraines.
- Rashes or itching.
The adverse effects of immunotherapy generally end up being much less severe after the initial treatment.
Throughout treatment, the treatment group provides encouraging treatment services, including nutritional assistance, naturopathic assistance, discomfort monitoring, oncology recovery, behavioral health and wellness, and spiritual support. These treatments might help in reducing negative effects and boost the individual’s general quality of life during immunotherapy.
Types of immunotherapy
The goal of immunotherapy is to attempt to reset the body’s immune system to once again have the ability to discover and attack cancer cells. The many kinds of immunotherapies work in different ways and have their very own dangers and advantages. Which of these therapies the care team advises depends on the type of cancer cells and their stage.
- Monoclonal or restorative antibodies: These are expanded in a laboratory and injected into the body. Some mark cancer cells so the immune system is able to recognize and destroy them. Others are extra direct in their approach, stopping the development of cancer cells or triggering their self-destruction.
- Adoptive T-cell therapy: It goes by several names– consisting of adoptive cell treatment, adoptive immunotherapy, or immune cell treatment. Essentially, the treatment group harvests leukocytes from inside the tumor and expands them in a laboratory, making changes to reinforce the natural capacity to fight cancer cells. These cells are expanded in huge batches and infused back right into the body to combat the cancer.
- Immune checkpoint inhibitors: These are a sort of medication that removes natural barriers within the body that keep the immune system in check. Without these all-natural blockades, it might overreact– like in autoimmune illness. However, cancer cells frequently use these clogs, or healthy proteins, to evade the body’s immune system. With these clogs deactivated with checkpoint inhibitors, the door is opened, and the body can respond more strongly to the cancer cells.
- Cancer cell vaccines: Also called immunotherapeutic or therapy injections, improve the immune system when the patient currently has cancer cells. They aren’t preventative vaccinations like those for infections, such as the flu. By supplying immune cells with a target discovered on cancer cells, they prime the body to produce antibodies to strike cancer cells. Injections usually consist of an immune-stimulating agent to rally the leukocyte troops, particularly against that protein target.
- Cytokines: These are healthy proteins produced by the body during natural infections that play a crucial role in stimulating the immune system cells. By supplementing the body’s all-natural cytokines with variations developed in research laboratories, these therapies assist in ramping up immune cells and relocating them toward their target: the tumor.
- Body immune system modulators: They are often called immunomodulators, and are medicines that ramp up the body’s immune reaction. Various immunomodulators act in various ways– some focus particularly on certain parts of the immune system, while others act across the entire body.
- Immunotherapy might be provided as an IV medicine right into the capillary, an oral medicine in tablets or pills, or even a topical medication on the skin.
Immunotherapy vs. chemotherapy
Both immunotherapy and chemotherapy are typically used cancer therapies that utilize medications to stop or slow the growth of malignant cells. Nevertheless, while radiation treatment medicines are used to attack swiftly growing cells throughout the body, immunotherapy activates the body’s immune system’s capacity to identify and attack cancer cells.
The negative effects can be extremely different between radiation treatment and immunotherapy, as well. Because chemotherapy can’t distinguish between the cells it’s targeting, it affects both fast-growing malignant and fast-growing regular cells, like those responsible for hair and skin development, and those lining the digestive system and creating bone marrow. That is why side effects like loss of hair, nausea and vomiting, and skin and nail changes are much more common and occasionally extreme with radiation treatment.
Benefits of immunotherapy

In general, immunotherapies are still less common than surgery or chemotherapy to deal with cancer cells. But also for some sorts of cancer, these therapies are currently a vital therapy choice. Many other immunotherapies are still in medical trials.
Immunotherapies have the potential to be more extensive and less toxic than other types of treatments for cancer, because they harness the power of the body itself to strike the growth as opposed to introducing chemicals into the body.
Immunotherapies are a really active area of research in cancer treatment, and brand-new treatments remain to be approved.
Also Read: Immunotherapy for cancer: How it works, who’s a candidate, and where to get it.
Risks of immunotherapy
Risks vary by the kind of immunotherapy, the kind of cancer cells, the stage, a patient’s general health and wellness, and the current therapy regimen. Every therapy has various side effects, and people may respond in a different way to the exact same treatment.
Generally, side effects may result when a client’s immune system ramps up to operate on “high.” When an individual obtains a vaccine, he or she might experience flu-like signs– including high temperature, cools, weak point, dizziness, nausea, muscle mass pains, fatigue, or frustration– because the body’s immune system is doing its task.
These therapies may trigger high degrees of inflammation in healthy cells and tissues and adverse effects from that response, such as a skin breakout. Steroids may treat the negative effects of that inflammation; however, steroids additionally have some side effects of their own.
Some individuals establish resistance to immunotherapy. Hardly ever have physicians actually observed severe or even fatal allergic and inflammatory reactions to some sorts of immunotherapy.
The person’s body may or might not respond to immunotherapy. Just some people receiving these treatments react to them. Scientists are dealing with better understanding the typical web link between people that do react and why.
Ask the treatment team about the threats and advantages of immunotherapy for the client’s kind and stage of cancer cells.
Also Read: What’s new in cancer immunotherapy?
What is the success rate for immunotherapy?
Between 20 percent and 40 percent of individuals who are provided immunotherapy mount an action against the medications.
Who is a candidate for immunotherapy?
Participants of the client’s multidisciplinary care group collaborate to develop treatment choices tailored to each person’s individual cancer care requirements. Immunotherapy treatment may be an alternative for people who have certain types of cancer cells. The therapy may work better for some kinds of cancer than others, so the individual’s oncologist would carefully monitor his/her progress and may suggest that immunotherapy be used in combination with various other therapies.
As soon as the care group creates a preferred treatment strategy, participants spend the time required with the client and his or her caretaker to explain each choice, its possible risks and benefits, side effects, and other fundamentals. After that, the client and his/her treatment team work together to make a decision which immunotherapy or various other treatment choices are right for him or her, allowing for informed choices about the treatment strategy.
Also Read: Immunotherapy Drugs for Cancer
Also Read: Can Immunotherapy Cure Stage 4 Cancer?
- Liver Cancer Diet Plan: Best Foods to Eat & Avoid During Treatment
- How Immunotherapy Empowers the Immune System to Defeat Cancer?