Why Cancer Is Rising in India: 15 Hidden Factors You Should Know
Cancer, a word that evokes fear worldwide, is becoming increasingly prevalent in India. Over the past few decades, the country has experienced a troubling rise, with nearly 15 lakh new cases diagnosed each year, and the numbers continue to grow steadily, making it a major public health issue. Even more concerning is how quickly cancer is spreading across different age groups, regions, and socioeconomic backgrounds. This article explores 15 alarming yet critical factors driving the increase in cancer in India.
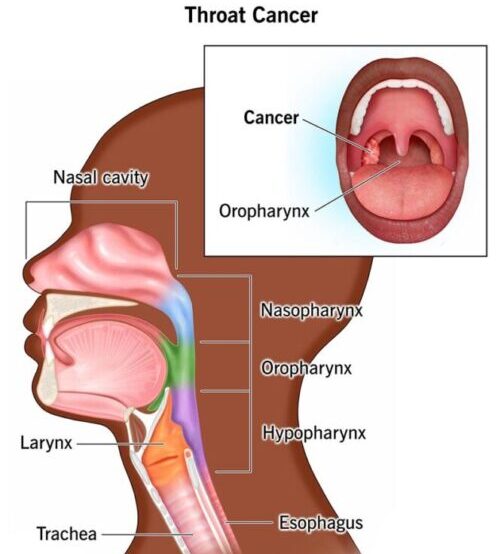
1. Tobacco and Alcohol Use
Because of the widespread use of tobacco, India accounts for nearly one-third (about 30%) of all oral cancer cases globally. Tobacco use, which includes chewing gutkha and khaini (in rural areas) as well as smoking cigarettes and bidis (in urban areas), continues to be the nation’s leading preventable cause of cancer.
Apart from this, the alcohol used in combination with smoking increases the risk of esophageal, liver, and breast cancers.
2. Air Pollution and Carcinogens
One of the major factors contributing to the increased risk of cancer is environmental pollution.
- Air Pollution: Megacities like Delhi and Mumbai regularly record poor Air Quality Index (AQI) levels. Fine particulate matter (PM2.5) has been strongly linked to lung, nasal, and bladder cancer.
- Water Contamination: Untreated industrial and toxic waste is being dumped in water bodies such as the Yamuna in Delhi, contaminating water supplies, especially in industrial belts.
- Radiation and Heavy Metals: Long-term exposure to arsenic, lead, and UV radiation also increases cancer risk.
3. Sedentary Lifestyle and Screen Time
The advancement of digital technology has led to a decline in in physical activity, even among children. Together with poor diets, this unhealthful behavior leads to obesity, diabetes, and inflammation.
Some studies suggest that obese people are at a higher risk of developing 13 different types of cancer.
4. Dietary and Lifestyle Changes
India’s eating habits have changed significantly. Fast food, sugary drinks, and highly processed foods are replacing traditional, nutrient-dense diets. These foods frequently contain trans and saturated fats, preservatives, and artificial colors, all of which are linked to cancer.
When combined with sedentary behavior, these habits can lead to obesity, diabetes, and metabolic syndrome—all of which increase cancer risk.
5. Urbanization and Stress Levels
Long-term stress and long working hours, along with poor sleep, can disrupt hormonal balance and impair immunity. Prolonged stress can result in unhealthy habits like drinking, smoking, and overeating, all of which increase the risk of cancer.
Although stress does not directly cause cancer, it can accelerate the growth of tumors by weakening the body’s defenses (immunity).
6. Late Diagnosis and Poor Screening Rates
Many cancers are curable in their early stage if detected early. Sadly, in India, over 70% of cancer cases are diagnosed at Stage III or IV, when chances of survival are relatively low. This is due to
- Limited Cancer screening programs.
- Lack of public awareness of cancer
- Lack of access to healthcare, particularly in rural areas
7. Family History and Genetics
While environmental or lifestyle factors account for 80-90% of cancer of all types, 5-10% of cancers are inherited (passed down through families). Due to a lack of knowledge about genetic counseling and screening in India, high-risk families miss out on early prevention opportunities.
8. Role of Infections and Viruses
Certain viruses are known to cause cancer:
- Human Papillomavirus (HPV) causes cervical cancer, one of the leading causes of death among Indian women.
- Hepatitis B and C viruses are associated with liver cancer.
- Helicobacter pylori infection raises the risk of stomach cancer.
Vaccination, such as for HPV and early infection treatment, can help prevent many of these cases.
9. Radiation from Gadgets & Medical Devices
Still under investigation, exposure to low-grade radiation from cell phones, Wi-Fi routers, and repeated high-dose imaging during medical scans may raise the risk of long-term cancer and cause cellular damage.
Sources:
10. Hormonal and Reproductive Factors
Modern reproductive patterns like
- Delays in getting married and having children
- Growing use of IVF and oral contraceptives
- Late menopause and early menstrual onset
They are found to be linked to higher risks of breast and ovarian cancer in women.
11. Occupational Exposure to Carcinogens
Due to exposure to hazardous materials, workers in industry and agriculture are at a heightened risk of developing cancer. Farmers often use pesticides like organophosphates and DDT—known carcinogens—without protective gear. Similarly,
Workers in the industrial sector are exposed to silica dust, benzene, and asbestos. Poor safety regulations and a lack of protective equipment cause long-term health hazards in both sectors.
12. Lack of Healthcare Access
Due to the poor coordination and lack of integration, India’s healthcare system is heavily fragmented:
- Rural areas lack diagnostic facilities.
- Private hospitals are too expensive for the average citizen.
- Government hospitals often face overcrowding and long wait times.
This results in significant delays in diagnosis and treatment.
13. Social Stigma and Lack of Cancer Awareness
Cancer is still considered a death sentence in many Indian communities. Patients often delay visiting doctors due to
- Shame and stigma are linked with breast and cervical cancers (in women).
- Cultural stereotypes and a lack of open discussion regarding reproductive health may lead to late detection and poor results.
- Strong faith in spiritual or alternative therapies often causes patients to ignore or put off evidence-based medical care.
- Misinformation and false fears about the side effects of chemotherapy and radiation discourage many from getting proper care.
- The lack of affordable, trustworthy health education allows myths and disinformation to spread, especially in rural communities.
Knowledge about cancer, together with proper screening and timely testing, can make all the difference.
14. Poor Food safety regulations
In India, carcinogens like BPA, formaldehyde, and lead are often found in contaminated cosmetics, tainted food, and unregulated packaging materials.
15. Government Policies and Public Health Gaps
India has launched several initiatives, including the National Programme for Cancer, Diabetes, Cardiovascular Diseases, and Stroke (NPCDCS). However, challenges still exist due to
- Shortage of funds restricts their outreach, infrastructure, and impact, particularly in rural areas.
- Poor implementation of the program, lack of communication, and lack of trained staff, leading to limited monitoring.
- absence of nationwide screening required for early detection and timely treatment
To reverse the trend, a stronger and more proactive policy approach is required.
Effective Strategies to Reduce Cancer Burden in India
Cancer rates in India are rising not only due to lifestyle changes but also due to a combination of biological, environmental, social, and economic factors. To combat this growing crisis, a comprehensive strategy based on prevention, early detection, and equitable access to affordable treatment is required.
- Nationwide Awareness programs: India needs to spend money on broad, multilingual campaigns that use social media, radio, television, and local outreach to inform people about risk factors, early warning signs, and the value of immediate medical attention.
- Education on Cancer Prevention: Cancer prevention education should start early. Schools and colleges can run age-appropriate health programs that cover topics such as tobacco avoidance, safe sexual practices, healthy eating, and recognizing symptoms.
- Compulsory Screening for High-Risk Groups: Government and healthcare providers should conduct regular screening for high-risk groups—like women over 40 (for breast and cervical cancer) and heavy smokers or drinkers (for oral and lung cancer)—to identify the disease in early stages when it’s most curable.
- Improved Healthcare Infrastructure: Diagnostic tools, cancer specialists, and basic healthcare access are frequently unavailable, particularly in rural communities. Setting up mobile screening vans, telemedicine, and cancer treatment clinics in these areas can significantly increase survival rates.
- Cancer Treatment Schemes and Insurance: By making cancer treatment affordable through government-funded insurance schemes like Ayushman Bharat, we should include more comprehensive cancer care services, reducing the financial pressure on middle- and low-income families.
- Regulating Toxic Pesticides and Tobacco: Strict regulatory policies on carcinogenic substances like gutkha, cheap bidi cigarettes, and hazardous pesticides are important. Similarly, encouraging organic farming and tobacco de-addiction programs can further reduce exposure.
- Promoting Healthy Diets and Habits: Obesity and other long-term conditions linked to cancer can be prevented with the support of national programs that support traditional Indian diets, daily exercise, and routine health examinations. This includes school meal reforms and workplace wellness initiatives.
Conclusion
The increase in cancer cases in India serves as a warning to citizens, legislators, and medical professionals. Strong public health policies, early detection, prevention, and awareness are the only ways to fight this silent epidemic. Understanding why cancer is increasing in India is the first step. Acting on this knowledge is the next step.
Overview: India vs Global Cancer Trends—Key Differences, Causes & Strategies
| Category | Global Trends | India-Specific Trends |
| Annual New Cases | ~20 million (GLOBOCAN 2020) | ~1.5 million (ICMR-NCDIR 2023) |
| Most Common Cancers | Breast, Lung, Colorectal | Breast (women), Oral & Cervical (high tobacco/HPV prevalence) |
| Top Risk Factors | Tobacco, obesity, aging, alcohol, HPV | Tobacco (30–35% cancers), air pollution, poor hygiene, and late diagnosis |
| Tobacco-Related Cancer Share | ~22% | ~30–35%, especially oral and lung cancers |
| HPV Vaccination Coverage | 80–90% in developed nations (routine in schools) | <10%, vaccine introduced only recently (Cervavac) |
| Access to Screening | Routine mammograms, colonoscopies, and pap smears are in place | restricted screening programs, mostly in metro cities |
| Cancer Stage at Diagnosis | 40–50% diagnosed early in developed countries | Over 70% diagnosed in Stage III or IV |
| Survival Rate (Breast Cancer) | 85–90% in developed countries | ~60%, due to late diagnosis and treatment access issues |
| Healthcare Investment | High investment in oncology (e.g., >7% of health budgets in EU/USA) | <2% of the national health budget is allocated to cancer care |
| Cancer Registry Coverage | >70% of the population (developed nations) | ~15–20% of the population (India), limiting data quality |
| Common Environmental Exposures | Air pollution, processed food, and radiation | High air pollution, pesticide exposure, and unsafe drinking water |
| Occupational Risk Factors | Regulated (e.g., asbestos ban, industrial safety standards) | Poorly regulated; high exposure to asbestos, silica dust, and toxic chemicals |
| Public Health Initiatives | Strong nationwide screening, vaccination, and early detection programs | NPCDCS was launched, but underfunded and poorly implemented in rural areas |
| Tobacco Control | Strict tobacco laws and taxation in many countries | Enforcement is weak; tobacco is still widely available and marketed |
| Cancer Prevention Strategies | Public education, early screening, lifestyle changes | Awareness campaigns are increasing, but need more grassroots-level interventions |
| Radiotherapy/Chemo Access | Standard across regions in high-income countries | Limited in Tier 2/3 cities; rural access is quite low |
Key Points:
- India’s cancer burden is increasing more quickly than the global average. Due to the poor healthcare system in rural areas, lifestyle and environmental factors, and late detection,
- India has higher rates of air pollution, tobacco use, and cervical cancer linked to HPV than many developed nations.
- Affordable treatment, public awareness, and early screening continue to be the most important gaps that India needs to close.
FAQs
Why is cancer increasing in India?
Tobacco use, air pollution, poor diet, low screening rates, infections like hepatitis and HPV, and genetic predisposition are all contributing factors to the rise in cancer cases.
Which type of cancer is most prevalent in India?
While lung and oral cancers are more common in men, breast cancer is more common in women.
Is it possible to prevent cancer?
Indeed. Up to 40–50% of cancers can be avoided with early screening, immunizations, and lifestyle modifications.
What age group is most affected by cancer in India?
The majority of cases occur in adults aged 40 to 65, but cancer is also becoming more common in younger populations due to lifestyle factors.
Is cancer hereditary?
Although some cancers run in families, the majority are caused by environmental and lifestyle factors. Genetic testing can help you understand your risk.