Diabetes and Cancer: How High Blood Sugar Raises Risk
Diabetes and cancer—two of the most serious global health burdens—may seem unrelated at first glance. However, increasing evidence demonstrates a strong connection between them. If you’re living with diabetes, especially Type 2, your risk of developing certain types of cancer is significantly higher. But what’s the link? And more importantly, what steps can you take? This article explains how diabetes increases cancer risk, the mechanisms involved, and how proactive health management can lower this double threat.
What Is Diabetes?
Diabetes is a chronic condition in which the body struggles to control blood sugar (glucose) levels. Glucose, the body’s main energy source, needs insulin—a hormone made by the pancreas—to get into cells. When insulin production is low or the body becomes resistant to insulin, glucose builds up in the blood. Over time, high blood sugar can harm the eyes, kidneys, nerves, and heart and can also increase the risk of cancer.
Two Main Types of Diabetes
- Type 1 diabetes: It is an autoimmune disease in which the body targets the pancreatic cells that produce insulin. It’s less common and usually diagnosed early in life.
- Type 2 Diabetes: The most common type (90-95% of all cases) is frequently associated with lifestyle choices. The body either produces insufficient insulin or develops resistance to it.
Diabetes is on the rise worldwide.
According to the International Diabetes Federation (IDF), 537 million adults worldwide were living with diabetes in 2021. This number is projected to increase to 783 million by 2045. With these alarming estimates, the ripple effects—including the risk of cancer—warrant serious attention.
Why Do People Develop Diabetes?
- Type 1: Genetic factors and environmental triggers (e.g., viruses) cause autoimmune destruction of insulin-producing beta cells.
- Type 2: Caused by a combination of genetics and lifestyle choices, including poor diet, physical inactivity, and obesity.
Diabetes warning signs
Recognizing early symptoms is critical. Watch out for:
- Frequent urination, particularly at night.
- Extreme thirst.
- blurry vision
- Wounds that heal slowly
- Unexplained weight loss
- Fatigue
- genital itching or frequent infections
Screening and Diagnostic Tests
If you are overweight, inactive, or over the age of 35, you should get an early screening. Common tests include the following:
- Hemoglobin A1C Test: Reflects average blood sugar over 2–3 months
- Fasting Blood Sugar: If your Diabetes level is ≥126 mg/dL
- Glucose Tolerance Test
- Random Blood Sugar
- Autoantibody tests (for Type 1diabtetes)
- Gestational diabetes screening during pregnancy
How Diabetes Increases Cancer Risk?
Multiple studies have confirmed a strong link between diabetes and cancer. Type 2 diabetes, in particular, is associated with an elevated risk of:
- Liver cancer
- Pancreatic cancer
- Colorectal cancer
- Endometrial cancer
- Breast cancer
- Bladder cancer
Here’s how the risk plays out:
- Diabetes increases the risk of liver and pancreatic cancer by up to twofold.
- Women with diabetes and breast cancer have a higher death rate.
- Prostate cancer risk in men is complex and varies by cancer aggressiveness, with ongoing research an anomaly that is still being investigated.
What’s the Biological Link?
Diabetes and cancer share common risk factors and mechanisms:
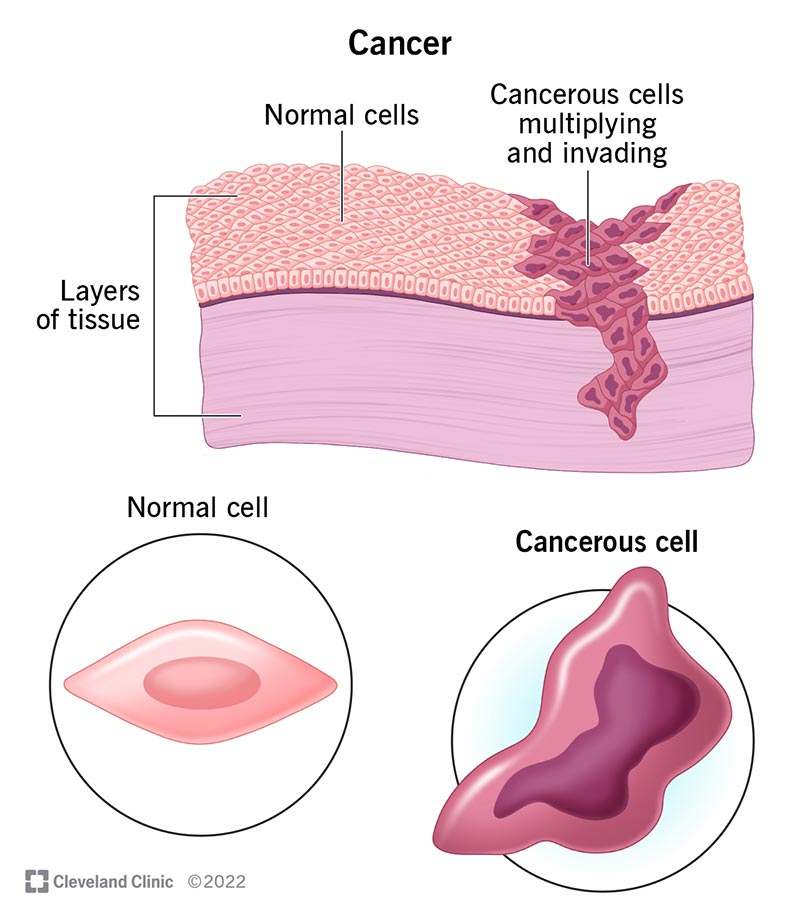
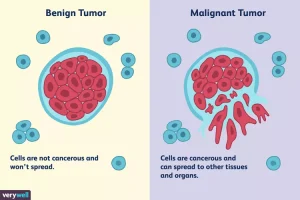
- Insulin Resistance and Hyperinsulinemia: Too much insulin in the blood can stimulate the growth of tumors by acting as a growth factor.
- Chronic Inflammation: Diabetes and obesity lead to low-grade, persistent inflammation, which provides the perfect conditions for the growth of cancer cells.
- High Blood Sugar: Because cancer cells are glucose-hungry, they can consume significantly higher amounts of sugar more quickly than healthy cells. This is why PET scans use glucose to detect tumors.
Can Diabetes Medication Reduce Cancer Risk?
A popular medication for diabetes called metformin is being researched for possible anti-cancer effects. According to research, metformin:
- Limits the amount of glucose that cancer cells can access.
- It may lower the mortality and incidence of cancer in diabetic patients.

The opposite is also true: diabetes can be brought on by cancer.
According to a 2018 study published in JAMA Oncology, diabetes is up to six times more common in cancer patients, particularly in the two years following treatment.
Causes Include:
- Steroids and chemotherapy raise blood sugar levels.
- Insulin-producing cells may be harmed by radiation therapy.
- Type 1 diabetes can be brought on by immunotherapy, such as checkpoint inhibitors.
- Type 2 diabetes is five times more likely to occur in people with pancreatic cancer.
This bidirectional relationship means that both diabetes and cancer must be managed together, holistically.
Diabetes Management During Cancer Treatment
It can be challenging to manage diabetes while receiving cancer treatment. Stress and side effects from treatment can result in dangerous drops in blood sugar (hypoglycemia) or spikes (hyperglycemia).
Signs of hyperglycemia:
- Too much thirst
- Frequent urination
- Vision blur
- Tiredness (fatigue)
Management of abnormal Blood sugar levels:
- Regularly check your blood sugar levels.
- Talk to your doctor about modifying your insulin or medication.
- Continue eating a balanced diet.
Hypoglycemia Symptoms:
- Shaking
- Confusion
- Sweating
- Dizziness
How to manage Low Blood sugar levels?
- Have some juice or sugary water.
- Take some glucose pills.
- Eat a small snack of carbohydrates.

Ways to Avoid Diabetes and Cancer
Diabetes prevention strategies also help to lower the risk of developing cancer. Aim for:
- Healthy Diet: Make up two-thirds of your plate with colorful vegetables, fruits, and whole grains. Also, limit your intake of red and processed meats.
- Exercise: Aim for 150 minutes of moderate or 75 minutes of vigorous exercise each week.
- Alcohol Moderation for Women: Max 1 drink/day, and Men Max 2 drinks/day
- Blood Sugar Control: Stay within target glucose ranges before, during, and after cancer treatment.
Diabeto-Oncology: A New Frontier
With an increase in comorbid cancer and diabetes, a new specialty called diabeto-oncology is emerging. It combines oncologists, diabetologists, and endocrinologists to offer:
- Individualized treatment plans.
- Early diabetes complications screening
- Biomarker-based preventative methods

Conclusion
Diabetes management during cancer treatment is challenging. Stress, side effects, and certain therapies can cause blood sugar swings, leading to hypoglycemia or hyperglycemia. Furthermore, certain cancers may cause paraneoplastic effects or directly interfere with metabolism, which would further impair glucose regulation. This reinforces the bidirectional link between diabetes and cancer, emphasizing the importance of careful, coordinated care.
FAQs
Can controlling diabetes reduce cancer risk?
Yes. Maintaining healthy blood sugar levels, weight, and lifestyle habits can significantly reduce the risk of developing cancer.
Is metformin effective in preventing cancer?
Emerging research suggests metformin may have anti-cancer effects, but more studies are needed before it’s used solely for cancer prevention.
Should cancer patients be screened for diabetes?
Absolutely. Cancer treatments can impact glucose metabolism. Early screening and management help prevent complications.