Childhood Brain Stem Glioma: Symptoms, Diagnosis & Treatment Guide
Although a child getting a brain stem glioma diagnosis can be deeply concerning, it’s crucial to remember that today’s medical advancements provide greater knowledge, early detection, and better treatment options. This article takes you through the main signs to look out for, the diagnosis process, and the most modern treatment with the right team, early intervention, and supportive care. Many families are discovering courage, clarity, and hope in the path ahead.
What is Brain Stem Glioma in Children?
Brain stem glioma is a rare and aggressive tumor of the brain stem, the area of the brain that connects to the spinal cord and regulates essential bodily processes like breathing, heartbeat, and motor skills. Usually, children between the ages of five and ten develop these tumors.
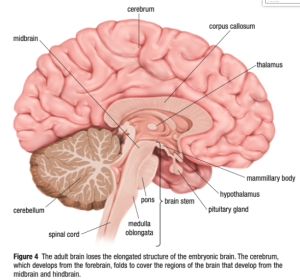
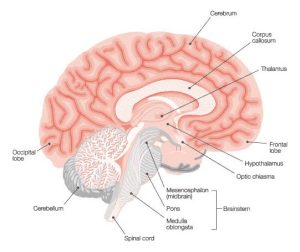
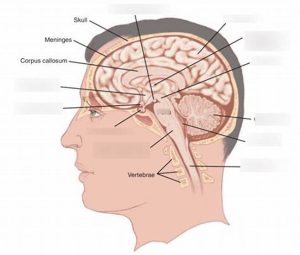
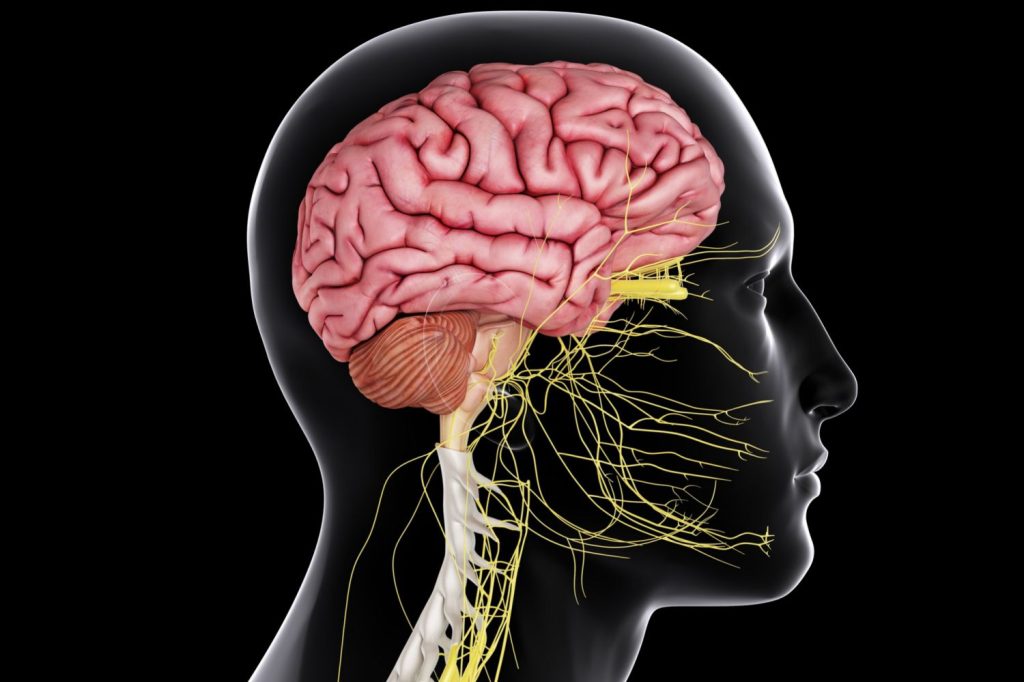
Anatomy of the Brainstem
The brainstem has three parts:
- Midbrain—Controls eye movement, hearing, motor control, and other functions.
- Pons—The Most common site for gliomas; it manages breathing, hearing, and facial sensations.
- Medulla oblongata—Regulates heart rate, blood pressure, and swallowing. It’s essential for survival.
Types of Brain Stem Glioma
Brain stem gliomas are categorized into two main types:
- Diffuse Intrinsic Pontine Glioma (DIPG): The most common and aggressive type affects the pons, especially in children
- Diffuse Brainstem Gliomas: High-grade gliomas spread aggressively throughout the pons and are surgically inoperable.
- Focal Glioma: Lower grade and slower-growing. Commonly found in the midbrain and medulla, they have a better prognosis.
Note: While gliomas commonly occur in the pons, it is not the only part of the brain stem, and the behavior of the tumor can vary depending on the location in the brain stem.
Signs & Symptoms of Brain Stem Glioma
Brain stem glioma symptoms in children may include:
- Double vision or problems with eye movement
- Facial palsy, or drooping face
- Speech or swallowing difficulties
- Arm or leg weakness
- Troubles with walking and balance
- Vomiting and headaches
Note: In case of persistent symptoms, consult your pediatric neurologist
What Causes Brain Stem Glioma in Children?
The exact cause is unknown, and they may appear suddenly without any reason. Below are some of the genetic conditions that may increase the risk:
- Neurofibromatosis type 1 (NF1)
- Li-Fraumeni syndrome
- Tuberous Sclerosis Complex
- Turcot syndrome
While most cases occur spontaneously without any identifiable cause, some known risk factors may increase the likelihood of developing the condition, including:
Age: Adults between the ages of 45 and 65 are most frequently diagnosed with gliomas. But they may occur at any age. Children and young adults are more likely to show certain types.
Radiation Exposure: Glioma risk has been associated with exposure to ionizing radiation, such as that used in cancer treatments.
Family History: Gliomas can sometimes run in families, despite their extreme rarity. To find out how and whether genetic traits can be passed from parents to children, more research is required.
Tumor Grading & Classification
While there is no standard staging system for childhood brain stem glioma, these can be classified into:
| Tumor Type | Grade | Description | Treatment Implications |
| Diffuse Gliomas | High-grade | Most common. Aggressive, spreading widely in the brainstem. | Difficult to treat; often not surgically inoperable; radiation is standard. |
| Focal Gliomas | Low-grade | Localized, often confined to one part of the brainstem (midbrain/medulla). | Slower-growing and may be removed surgically; better prognosis. |
| Recurrent Tumors | Variable | Can return after initial treatment, occur locally, or occur in new regions. | May require a new treatment plan; options may include chemotherapy, radiation, or clinical trials. |
Diagnosis of Brain Stem Glioma
Common Tests Include:
| Test | Purpose | Use Case |
| MRI Scan | Produces detailed brain images using magnetic fields. | The most accurate and commonly used tool for initial diagnosis. |
| CT Scan | Uses X-rays to create cross-sectional images of the brain. | Sometimes used, but less sensitive than MRI. |
| Biopsy | Removal of a tissue sample for microscopic examination. | Rare in diffuse gliomas due to risk; used in focal cases or research. |
Notes:
- Because of its clarity and non-invasiveness, MRI is the gold standard for diagnosing brain stem gliomas.
- Although CT scans can help with preliminary evaluation, they are typically insufficient for a conclusive diagnosis.
- In diffuse gliomas, biopsies are generally avoided unless the tumor has unique features or is a part of a clinical trial.
- By verifying the type and grade of the tumor, a biopsy can help direct treatment for focal gliomas.
Childhood Brain Stem Glioma: Key Statistics
- Incidence: Approximately 13% of pediatric CNS tumors originate in the brainstem.
- Location: Around 75% occur in the pons.
- Survival Rate: Varies by type; focal gliomas have a better outlook than diffuse ones. The 5-year survival rate for all pediatric brain tumors is around 75%, but much lower for DIPG.
Treatment Options for Childhood Brain Stem Glioma
Childhood brain stem glioma treatment is highly personalized and is based on factors such as tumor type (diffuse or focal), exact location, genetic features, and the child’s overall health.
Radiation Therapy: The main treatment for diffuse brain stem gliomas, such as DIPG, is radiation therapy, which helps reduce tumor size and alleviate neurological symptoms.
Chemotherapy: It may be more effective in some genetic subtypes and is frequently used in clinical trials, particularly for DIPG type or in conjunction with radiation to control tumor growth.
Surgery: Only focal gliomas, where the tumor is localized and safely accessible, are typically considered.
Supportive and Palliative Care: prioritizes symptom alleviation and emotional support and enhances the quality of life throughout all phases of treatment.
A key thought
Although childhood brain stem glioma is a complicated condition, there is new hope thanks to developments in supportive care, imaging, and treatment. A child’s quality of life can be considerably enhanced by a personalized approach that is led by professional care and emotional support. For those affected to have better results and more promising futures, Early diagnosis, access to specialized centers, and ongoing research are key to creating better outcomes and brighter futures for affected families.
FAQs
How rare is brain stem glioma in children?
About 13% of childhood brain and spinal cord tumors are caused by this rare condition.
Can brain stem glioma be cured?
It may be possible to cure focal gliomas. Although diffuse types can be controlled, they are frequently incurable.
What are the early warning signs?
Early signs include changes in vision, balance issues, and difficulty swallowing, which are common early signs.
Is surgery always an option?
No. Because of the brainstem’s sensitive location, surgery is usually only an option for focal gliomas.
Where should I seek treatment?
A pediatric cancer center with neuro-oncology expertise is recommended.